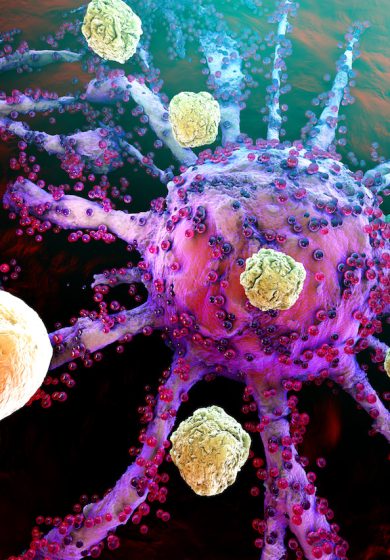
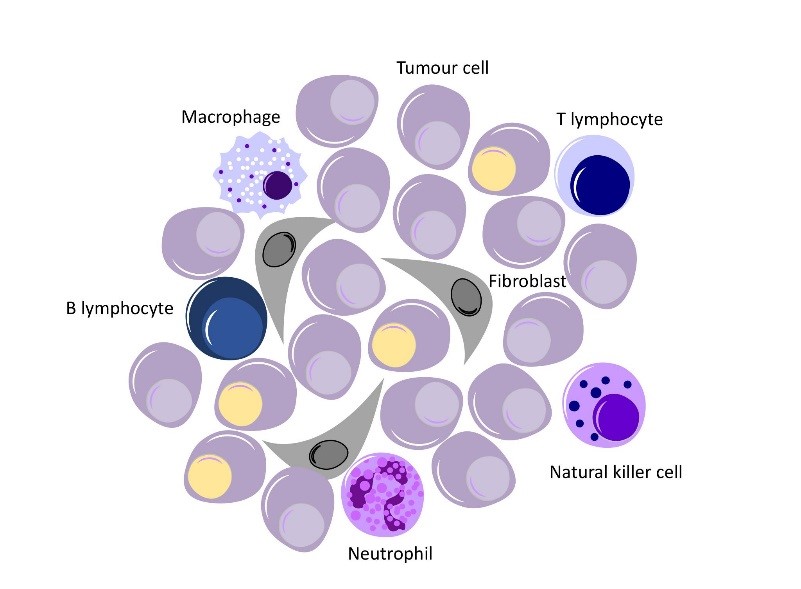
The immune system is the body’s defence mechanism to protect itself from harm. This harm can come from outside the body in the form of bacteria and viruses, and from inside the body, when cells, mutate or change to become cancerous. Our immune system is very complex and it is made up of many different types of cells, all of which work in different ways to protect the body. An example of one type of immune cell, is the cytotoxic T cell (aka T lymphocytes), which acts to protect the body by producing a chemical which causes foreign cells to kill themselves – leading to their death.
In recent years immunotherapies have emerged as a way to harness your own body to defeat cancer and generate a long-lasting response. Most of these therapies involve unleashing the T Cells to attack cancer cells and early successes have shown great results for certain cancers.
But while there have been great leaps forward, this powerful approach has only worked in 20-30% of patients. Although the immune system is more than capable of destroying cancer cells, it is also designed to avoid targeting the body’s own cells. Unfortunately, tumours have developed ways to hide from our immune system by exploiting the brakes the immune systems use to avoid killing healthy cells. So to get this powerful new treatment working for more cancer patients we must overcome the tumours’ manipulation of our immune system to get the immensely powerful immune cells to selectively target the cancer.
With your support, here are some of the ways Breakthrough scientists are working to find ways to ensure more patients can benefit from this approach.
Do B cells hold the key?
B-cells fight bacteria and viruses by making Y-shaped proteins called antibodies, which are specific to each pathogen and are able to lock onto the surface of an invading cell and mark it for destruction by other immune cells. B-lymphocytes and cancer have what may be described as a love-hate relationship. For example, B-cells sometimes prevent tumour development by producing antibodies that may attack cancer cells. Other times, regulatory B-cells may release immune-suppressive chemical (cytokines) that stifle an anti-tumour response. One of our research teams is studying regulatory B cells, to determine how best to stop their suppressive function. If they can block or remove this cell group, they hope to permit an immune anti-tumour response. This should result in the killing of tumour cells.
An electric pulse sparks the promise of better outcomes
Electrochemotherapy (ECT) has been pioneered in Cork thanks to funding from Breakthrough (and you!). It’s an emerging therapy for use in cancer tumours. ECT delivers short bursts of electricity to a tumour. That makes the tumour porous and dramatically increases the absorption of chemotherapy drugs. The electrical pulse has also been shown to spark an immune engagement against the cancer. A number of studies and trials are currently examining if this combination of ECT and immunotherapy can increase the number of patients it works for and who can have a long-term durable response.
Macrophages: these big eaters engulf and digest
We are learning more every day about tumour immunology. And a new range of therapeutic targets has opened up. Macrophages are cells that detect and destroy harmful organisms. But tumours can co-opt them to support tumour growth and defend against conventional cancer therapies. Our research team have been investigating the role of macrophages in prognosis and sensitivity to therapy. They are also exploring how we can change the behaviour of these cells in cancer patients.









 Contact
Contact